Credentialing 101: Empowering a New Era of Provider Accuracy and Trust
October 27, 2025 | by Steven Johnson

Why Provider Credentialing Is Critical in Modern Healthcare
Introduction
Provider credentialing is the foundation of patient safety and quality assurance in healthcare. As regulatory requirements evolve, healthcare organizations in 2025 face increasing scrutiny to verify credentials, maintain compliance, and streamline their onboarding processes. Credentialing ensures that physicians and advanced practice providers meet established standards before treating patients or billing payers, protecting organizations from costly mistakes, penalties, and reputational harm.
What Is Provider Credentialing and Why Is It Vital?
Provider credentialing is a multi-step, comprehensive review to confirm a practitioner’s academic achievements, training, board certifications, medical licenses, professional history, and reputation. As part of this process, organizations check for any malpractice claims, disciplinary actions, or gaps in employment to ensure the utmost reliability and competence.
Without thorough credentialing, organizations risk government and commercial payer penalties, audits, exclusion from networks, denied claims, and even legal action. Credentialing not only satisfies insurance and regulatory demands—it builds trust with patients and demonstrates organizational integrity.
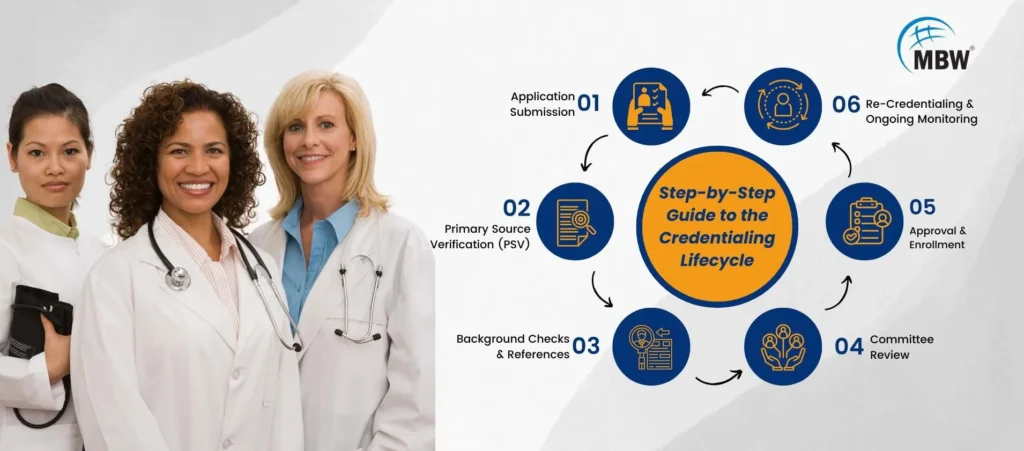
The Credentialing Process: How It Works Today
Credentialing begins as soon as a provider is hired or contracts to practice. The process involves obtaining and verifying countless documents—medical school transcripts, postgraduate training certificates, board certifications, state licenses, malpractice insurance, employment history, personal references, and background check results. Most healthcare organizations now use digital systems to streamline this paperwork.
Credentialing applications are submitted to payers, licensing boards, and hospitals. Information is then verified directly with issuing sources—such as medical schools, licensing boards, and professional societies. Modern platforms like CAQH and PECOS simplify these steps, but require constant updates and accuracy.
After initial verification, organizations perform exclusion checks with federal databases, search for open sanctions, and confirm that providers have no legal or financial barriers to practice. Peer review processes often evaluate providers’ clinical skills and professionalism.
Credentialing can take weeks or even months. Delays are common if documents are missing, information is inaccurate, or payers have unique requirements. Only after complete credentialing can providers begin seeing patients and submitting claims.
Recredentialing and Ongoing Monitoring
Credentialing is not one-and-done. To stay compliant, healthcare organizations must track credential expirations, changing regulations, and new payer standards. Providers undergo re-credentialing every few years, with ongoing background and license checks to ensure no issues arise after their initial approval.
Modern healthcare organizations use credentialing software equipped with automated reminders and real-time exclusion monitoring, drastically reducing lapse risks and helping organizations stay ahead of audits or payer queries.
Challenges in Credentialing—and How to Overcome Them
Common obstacles include missing records, outdated licenses, incomplete applications, or slow responses from primary sources. Organizations may face issues if they allow providers to practice before full approval, risking claim denials and liability.
To conquer these challenges, organizations should start the credentialing process early—ideally several months before a provider’s planned start date. Providers should receive clear instructions about what documents are required, why the process matters, and the consequences of non-compliance. Credentialing staff should keep lines of communication open with providers and payers, double-check applications for errors, and react promptly to requests for clarification.
Digitizing records and using credentialing software is especially valuable—reducing manual error, accelerating document management, and improving compliance monitoring.
Credentialing in Special Situations
Credentialing standards continue to change as telemedicine grows and new provider roles emerge. Remote providers, advanced practice clinicians, and facility-based staff often face additional documentation or multi-state credentialing requirements. Organizations should pay close attention to payer policies, evolving state laws, and accreditation standards to avoid surprises.
The Impact of Credentialing on Healthcare Organizations
Thorough credentialing brings rapid payer enrollment and reimbursement, protects revenue, and facilitates smooth onboarding. Organizations with streamlined credentialing processes gain faster network acceptance and reduce the risk of regulatory inquiry. Patients also benefit by knowing their caregivers have met rigorous standards for safety and professionalism.
On the other hand, organizations that neglect credentialing may face severe consequences—lost income, legal exposure, penalties, and damaged credibility.
Conclusion
Credentialing is a strategic priority in today’s healthcare environment. Its impact reaches from financial health to patient outcomes. By investing in proactive, accurate, and technology-driven credentialing practices, organizations can maintain compliance, attract top talent, and consistently deliver high-quality care.
Healthcare leaders should build strong credentialing protocols, educate their teams, and leverage new tools to simplify the process. Staying ahead of regulatory and payer changes is essential for ongoing success and growth. For more tips, credentialing webinars, and consulting tools, subscribe to our healthcare compliance updates.
RELATED POSTS
View all



