A Practical Guide to CARCs: Reducing Denials in Outpatient Medical Billing
October 6, 2025 | by Steven Johnson

A Practical Guide to CARCs: Reducing Denials in Outpatient Medical Billing
Outpatient denial management becomes far simpler when the ERA/835 is read as a unified message built from Group Codes, CARCs, and RARCs, each signaling responsibility, reason, and context for action. This guide shows exactly how to interpret that trio, implement CAQH CORE guardrails, and use electronic attachments to cut rework and accelerate reimbursement.
What CARCs are
Claim Adjustment Reason Codes explain why a claim or service line was paid differently than billed and are standardized within the X12 835 remittance advice, enabling consistent automation and review across payers. Group Codes like CO, PR, PI, OA, and CR assign financial responsibility for the unpaid amount, grounding posting and follow-up before any appeal work begins. Remittance Advice Remark Codes add specific context—often required for certain CARCs—so staff can correct or appeal with precision on the next cycle.
Why they matter
Standardized CARC/RARC usage improves automation, reduces rework, and speeds cash by clarifying what to fix and who should own it in denial work queues. Aligning denial queues to CARC categories makes triage faster and supports targeted training, coding feedback loops, and payer-specific appeal packets that actually overturn. Consistent ERA ingestion, acknowledgement, and reassociation also keeps funds and details synchronized, minimizing suspense and delays for secondary billing.
Read the code trio
Think of Group Code + CARC + RARC as a single instruction set: responsibility assignment, denial reason, and the extra detail to take the right next step, all delivered in the ERA/835 at both claim and line levels. Many CARCs expect companion RARCs, so complete ERA ingestion and mapping is essential to avoid guesswork and unnecessary appeals. When this trio is properly mapped into queues, preventable denials are fixed upstream while appealable items move with the right documentation on the first try.
Common denial drivers and fixes
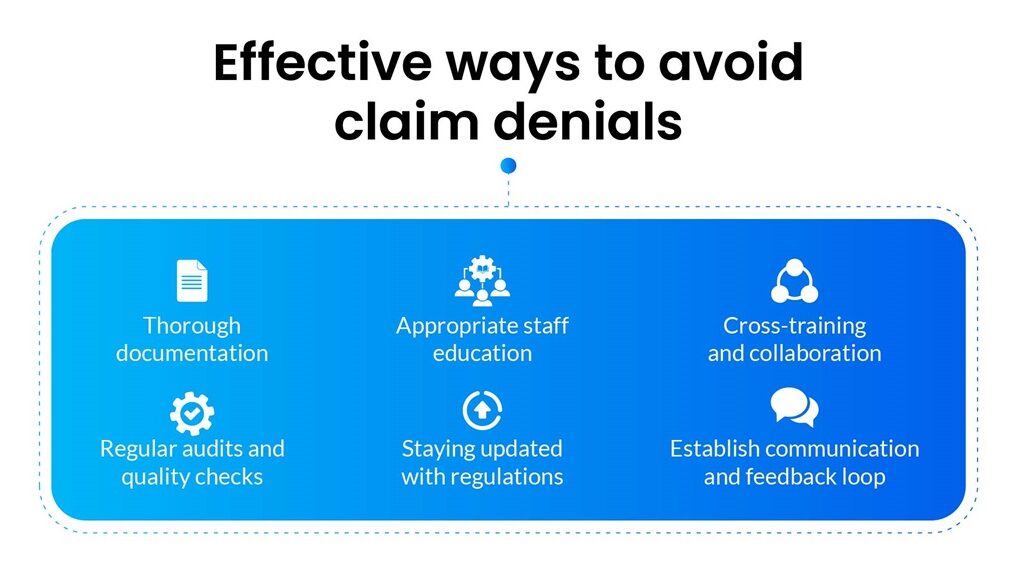
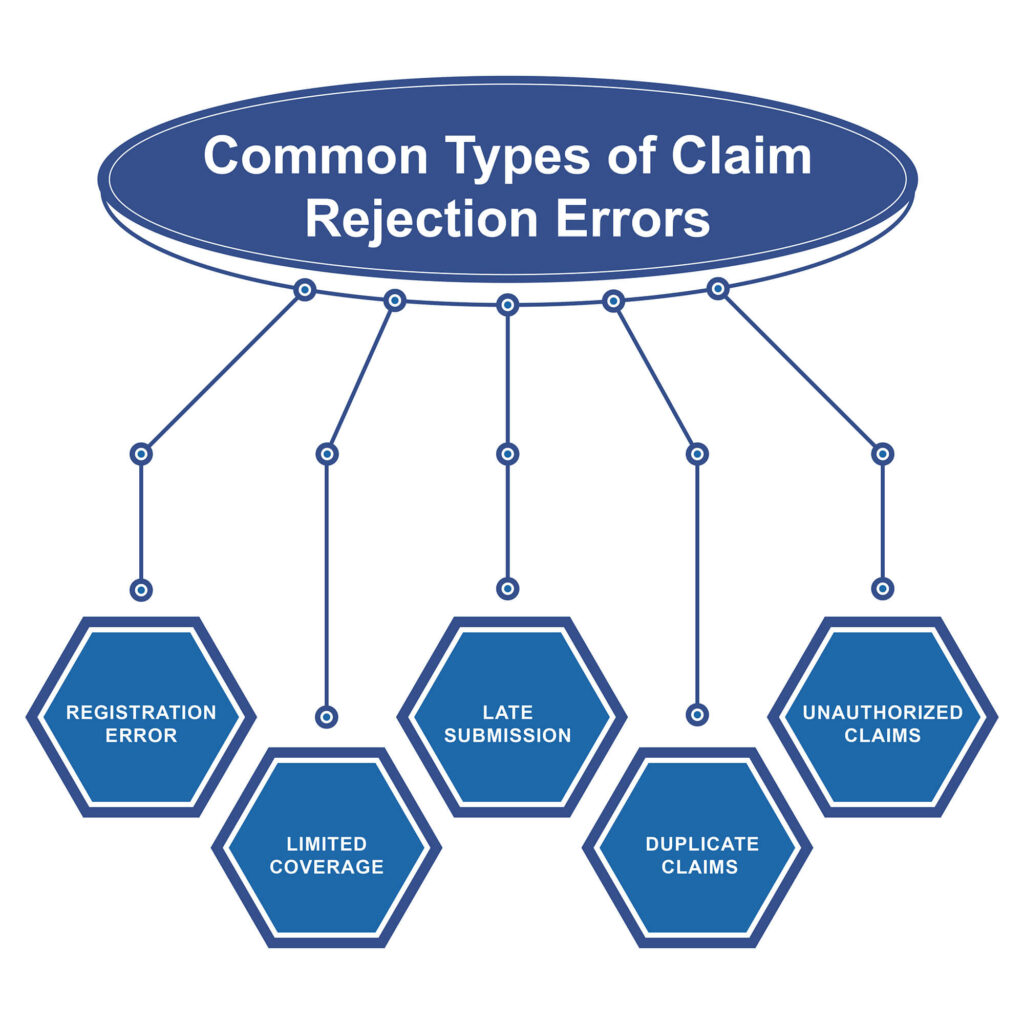
- Eligibility and coverage gaps frequently post under PR or PI, pointing to patient responsibility or payer-initiated reductions; strengthening scheduling-stage eligibility and COB checks reduces these repeat denials.
- Coding and bundling conflicts typically appear under CO or OA and respond to coding audits, fee schedule alignment, and consistent use of payer policies referenced in the ERA.
- Medical necessity and documentation shortfalls are often clarified by RARCs, so documentation checkpoints and timely attachments are critical in outpatient workflows.
- Prior authorization and referral issues drive CARCs like 197 and are best contained via scheduling-stage PA tracking and escalation SLAs.
- Timely filing rejections require payer-specific deadline tracking and queue SLAs to avoid avoidable write-offs.
- Duplicate billing flags such as CARC 18 are reduced by reconciling the ERA and claim control numbers before resubmission.
High-impact outpatient playbooks
- CARC 16: “Claim/service lacks information” Read the RARC for exactly what’s missing, correct, and resubmit promptly to protect filing windows; prevention hinges on pre-claim validation for identifiers, dates, codes, and required documents.
- CARC 197: “Precert/authorization/notification absent” Confirm if PA exists under another identifier, pursue retro if allowed, or appeal with clinical necessity and scheduling evidence; prevent with a service-level PA matrix and timers at scheduling.
- CARC 109: “Not covered by this payer/contractor” Correct payer routing, update coverage, and resubmit within deadlines; prevent through robust eligibility, COB prompts, and payer ID confirmation.
- CARC 18: “Exact duplicate claim/service” Reconcile ERA posting and void/correct before any resubmission; prevent by pausing resubmits until ERA/277 reconciliation completes.
- CARC 29: “Time limit for filing has expired” Appeal only with proof of timely filing; otherwise follow write‑off policy, and prevent with automated filing clocks and work queue SLAs.
- CARC 96/45 families: Non-covered or reduced to maximum allowable Split PR vs CO correctly and appeal only where policy or coding interpretation is defensible; prevent by keeping fee schedules and medical policies current and feeding trend education to coders.
ERA/835 guardrails that speed cash
The CAQH CORE 835 Infrastructure Rule sets common expectations like batch 999 acknowledgements and companion guide templates to stabilize ERA automation and mapping across payers. The CAQH CORE EFT/ERA Reassociation Rule requires proper use of the TRN reassociation trace number in the CCD+ Addenda Record, not the ACH trace field, ensuring payments and remits match reliably within the standard timeframe. Misplacing the trace number into the ACH trace field causes it to be overwritten by the bank under NACHA rules, breaking the linkage and creating suspense work that slows secondary billing and appeals.
Uniform CARC/RARC usage
Operating rules promote uniform CARC/RARC combinations and aligned companion guides, enabling higher auto-post rates and more accurate routing to denial queues by reason and responsibility. Maintaining parity with the CAQH CORE companion guide format reduces interpretation errors and promotes consistent appeal triggers across plans and lines of service. These standards work hand in hand with the X12 code lists that define and update CARC and RARC semantics over time.
Attachments that unlock approvals
When denials cite missing documentation, the HIPAA X12 275 claim attachment lets providers send the exact clinical notes, images, or forms electronically for faster adjudication and fewer resubmits. Payer companion guides often specify file types, size limits, and timing expectations, with best practice to submit the 275 and claim in close sequence so adjudication proceeds without delay. esMD and 275 guides outline how to carry identifiers and required codes so attachments match correctly to claims or requests on the payer side.
Appeals that actually overturn
RARCs frequently include timelines or rights such as Medicare appeal windows, so follow remit instructions precisely and mirror documentation expectations in first-submission appeal packets. Build payer-specific templates for top CARC combinations to ensure required clinical notes, policy citations, and authorization proof are present from the start, cutting cycle time significantly. Monitor reassociation and acknowledgement timing to prevent funding-detail mismatches that can stall appeals or delay secondary billing.
Track denial rate, dollars at risk, top CARCs, overturn rate, and days to resolution segmented by payer, site, and modality to aim fixes where they pay off fastest. Add operational metrics like 999 acknowledgement success and CCD+/835 reassociation timing to keep cash posting smooth and minimize suspense. Weekly reviews should convert top CARCs into upstream changes in registration, coding, and scheduling to prevent recurrence in outpatient flows.
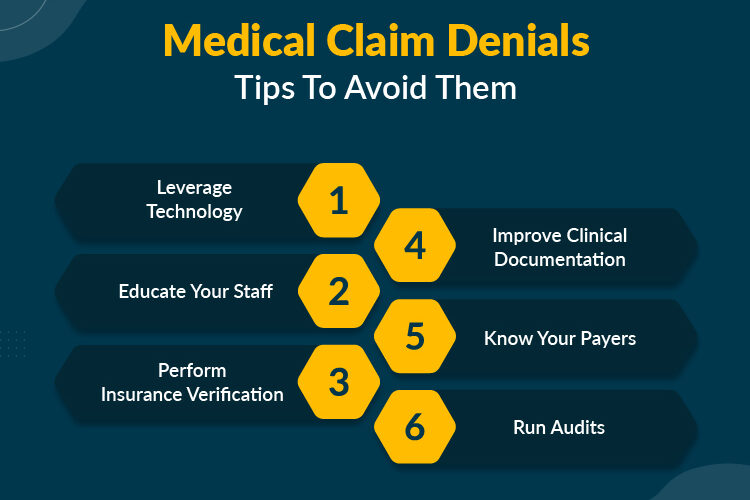
Quarterly refreshers should cover high-frequency CARCs, the companion RARCs they require, and payer updates so teams know exactly which documents and codes overturn specific denials. Operations, IT, and revenue cycle should align policies to CORE rules for acknowledgements, reassociation data, and dual-delivery expectations during onboarding and testing. Keep denial SOPs and mapping current with X12 code list updates so queues and analytics reflect the latest maintenance and payer practices.
| Group code | Responsibility notes |
| CO | Contractual obligation amounts the provider cannot shift to the patient under plan policy or contract terms, guiding correct posting and appeal scope. |
| PR | Patient responsibility elements such as deductible, coinsurance, or copay that should be billed to the patient or secondary in line with benefit design. |
| PI | Payer-initiated reductions outside the standard contract terms or for administrative reasons, often calling for policy review or appeal when disputable. |
| OA | Other adjustments that alter payment without assigning patient responsibility, frequently used for non-coverage or administrative changes. |
| CR | Corrections and reversals used to unwind prior transactions in legacy contexts; note usage constraints in newer versions. |
Quick wins checklist
- Turn on full ERA ingestion with CARC/RARC-to-queue routing and batch 999 acknowledgements to stabilize automation.
- Configure CCD+/835 reassociation using the TRN segment in the Addenda Record and monitor the standard reassociation window.
- Build mini playbooks for CARC 16, 197, 109, 18, 29, and 96/45 with required documents and payer-specific appeal templates.
- Enable X12 275 attachments for documentation-heavy services and RARC-directed requests.
- Add payer filing clocks and escalation SLAs to prevent avoidable write-offs tied to timely filing.
- Update companion guide mapping and staff training each quarter as code lists and CORE rules evolve.

Treat Group Code + CARC + RARC as a single operational command, then connect the insights to upstream fixes and electronic attachments so denials drop and appeals succeed on first pass. With CORE-aligned ERA operations, disciplined reassociation, targeted analytics, and payer-aligned appeal templates, outpatient teams can convert denials from a bottleneck into a predictable, fast-moving workflow. Staying current with X12 code maintenance and CAQH CORE rules ensures the program remains accurate and resilient as standards and payer practices change.
RELATED POSTS
View all